I work with clients who experience a wide range of mental, emotional, and relational health struggles. Some of those clients use medication as part of their wellness regimen. I am not a psychiatrist and do not prescribe medication. Therapists work with clients to be aware of how their medication is impacting symptoms. Research indicates that medication combined with therapy has the best outcomes compared to medication alone.
Psychotropic medicine…pharmaceutical support for conditions like depression, anxiety, bipolar, ADHD, etc…is a field with almost as many opinions as there are providers. SSRIs, SNRIs, tricyclics, mood stabilizers, stimulants, non-stimulants…there is so much we could get into here. I am in full support of clients using medicine to help support their mental health. Although there is controversy within the pharmaceutical industry, I believe there is enough evidence to support the benefit of medication to greatly improve a person’s quality of life and to reduce negative outcomes, including self-harm. Medication literally saves lives. It also makes a person’s life feel (to them) worth saving.
Frequently, a person will begin taking medication or has been taking medication for a while and report that although it is helping, it hasn’t made things completely better. It is completely normal for medication to help, but not completely remove the symptoms of a condition. However, this is when I get curious with clients.
Mental illness does not just affect a person’s mood or thoughts. It affects a person’s entire being. It affects hygiene, eating habits, sleep habits, energy levels, relationships, how a person moves their body, and so much more.
If a person has been mentally ill for a while there is a good chance that they developed habits and patterns based on how these areas of their life have been affected. Depression, anxiety, ADHD, Bipolar, and almost every mental health struggle affects circadian rhythms. People often have erratic sleep schedules, staying up late and struggling to wake up in the morning. Eating more or less. Hunkering inside and avoiding people or the sunshine. No motivation to move their body. Self-loathing and protective hypervigilance, which contributes to misinterpreting communication, isolating from relationships and/or falling prey to abusive dynamics. I often think about these associated behaviors as kind of coping “skills” used to try to survive being mentally unwell.
You will see Instagram posts citing research on how things like walking improve mental health. This is absolutely true. And. It isn’t quite as linear as social media would like for you to believe. It isn’t as simple as A+B=C. If I do this then I will not be depressed. It is much more difficult to determine what came first…the chicken or the egg. Does not walking and not being outside contribute to depression? Or does depression contribute to not walking or getting outside. The answer is probably…yes…both.
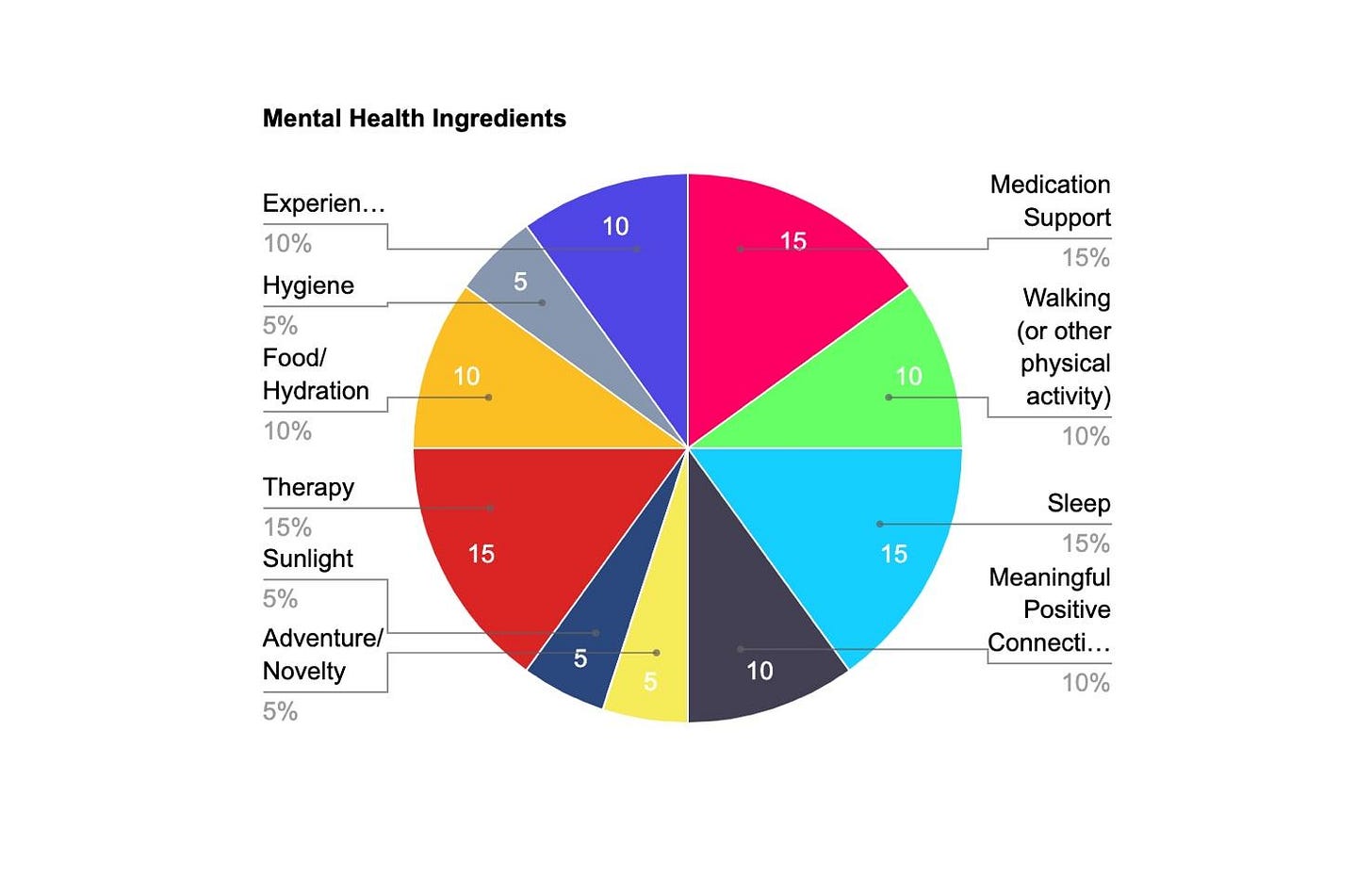
Recently when trying to conceptualize the way I think of treating mental illness, I ended up creating a pie chart. I used it to facilitate a dialogue with a client one day in session. It helped the client and me conceptualize how a variety of things contribute to our mental and emotional wellness just like a lot of different things contribute to our physical wellness. We were able to sit with it in a way that acknowledged all of the pieces involved…internal and external…individually and within their family and social context.
I then started using this same “pie chart” idea to talk with other clients who were experiencing chronic, often debilitating mental health struggles.
We talked about what contributes to mental health based on research, but also based on their own experiences. There was some psychoeducation involved. For example, some people do not realize that something like brushing your teeth and dental health is connected to mental health. Again, what came first, the chicken or the egg? In either case, mental health and dental health are correlated.
Here is one example of what that pie chart might look like with the following large category slices that I have gathered based on research and my 20 plus years of working with clients:
Medication support
Hygiene
Food/Hydration
Therapy/Personal Growth
Sunlight
Adventure/Novelty
Walking or some other physical activity
Sleep
Meaningful, positive connections
Experiences that make you feel competent/capable
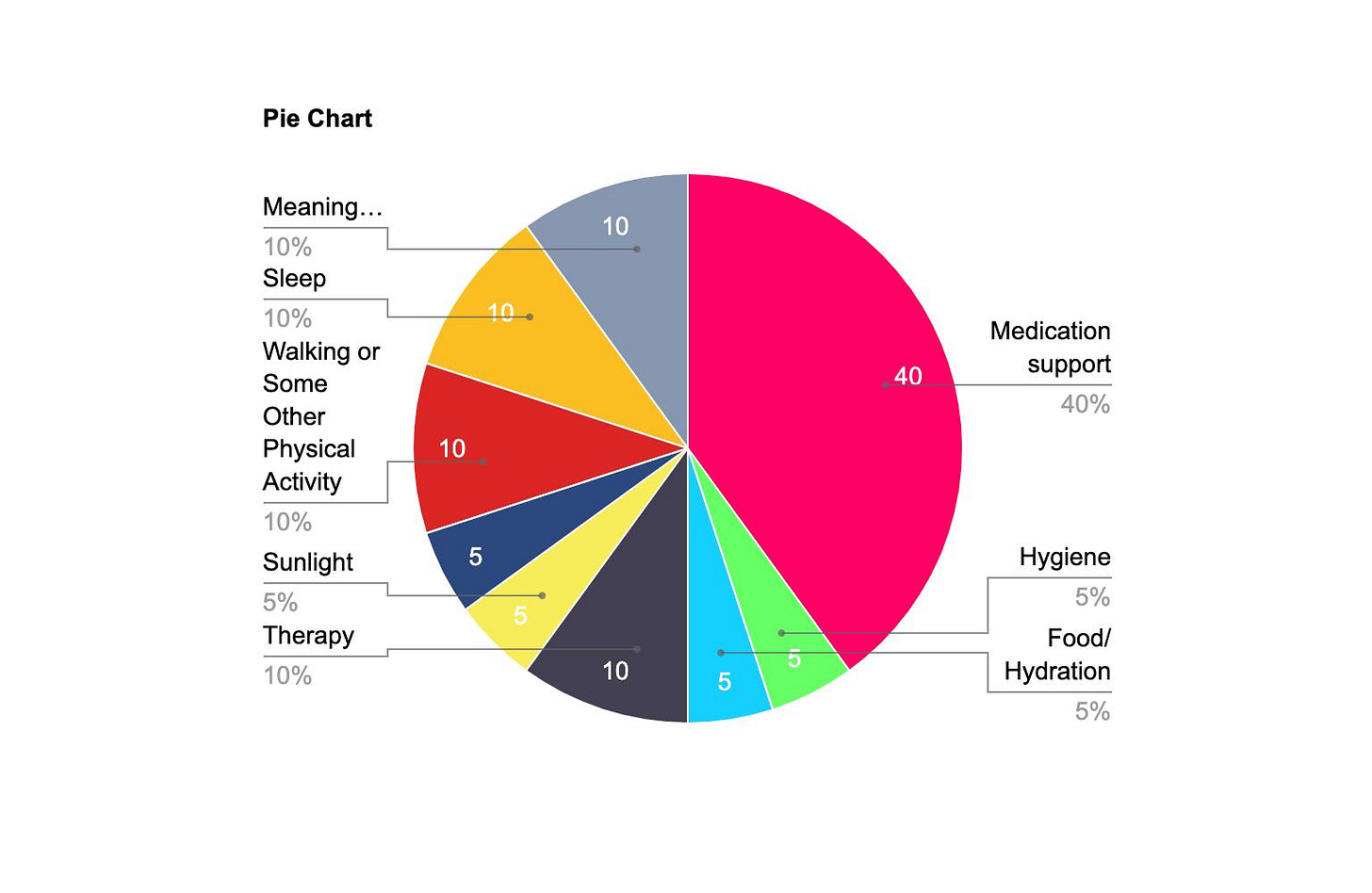
Or, maybe a person’s pie chart and the slices look like this.
Everyone’s pie can look different even if the ingredients are roughly the same.
So, a person might be diligent about taking their medicine, but that slice can only be so big. There is no way it can ever fill up the entire pie. The pie has more ingredients than just medicine. The same goes for any other ingredient to their mental health pie.
I sometimes use a scaling question to help clients talk about how they are feeling. On a scale of 0-10, with 0 being the worst you can imagine feeling and 10 you are living your best life, how are you feeling now? Then, I will ask what and when the lowest number was in the past week or two. What was going on then? Tell me the story around that point.
And, what was the highest number you experienced in the past week or two? Here is where I get really curious. What were the ingredients of the story at that point?
Time and time again I hear two pieces reported: competence and connection. They were doing something that made them feel good about themselves and their abilities and there were people around that made them feel seen, loved, cared for and/or respected.
The sense of competence doesn’t have to be anything huge. It can be from finally finishing a project at home or cleaning out a closet or feeling acknowledged at work or picking up a new or old crafting project.
So, how do we…how do you… inject those experiences into the life we live on a regular basis?
Another exercise I do to help clients get to know the ingredients of their pie is a very simple activity I learned in a training on treating trauma about 20 years ago. I call it “Red Light, Green Light”. You fold a paper so that you create three columns…like you are folding it to put into an envelope. Label one column “green light”, one column “yellow light” and one column “red light”.
Imagine life when it feels good. Things feel balanced and manageable. What kinds of things are present in your life?
For me, in my green light I am getting at least 7 hours of sleep each night. I am eating food that feels good for my body. I am reading books for fun and for work. I am getting a good balance between work, family time, and alone time. I am moving my body by walking, running, and lifting weights. I am connecting with friends on a regular basis. I am getting time to be creative and have little adventures. I am having experiences that make me feel good about myself such as a new training for work or cleaning out a closet.
Now, imagine when life starts to feel stressful. Things begin to feel overwhelming. What falls off the Green Light List and what gets added?
My sleep dips to under 7 hours a night. I reach for more sugary foods. I hole up or I go, go, go. I stop moving my body as much. And so on.
And, then when life feels…or you can imagine life feeling… in a crisis mode. Red light. What does that look like? What comes off the list and what gets added?
As I do this with clients, I will mentally go through the list myself. Our lists can change throughout our life and it is helpful for me to take a moment and consider my own lists and what life looks like for me, too.
Life will often feel “yellow light.” The idea isn’t that you can magically make life “green light” by engaging in the magical Green Light List. Still, we can look around, recognize the yellow light (or red light) stress and intentionally choose one item on the green light list to care for ourselves.
I think of it as a “self-parenting guide.”
Becoming an adult, in so many ways, is becoming your own parent. When you were little, your caregiver hopefully took you to the dentist and doctor. When you are an adult you take yourself to these appointments. As a child, your parent made sure you ate good food, got outside, had adventures, and fostered meaningful relationships. As an adult you step into the role of giving those things to yourself. Hopefully, when you were little you had a parent who could sit with you when you were upset and celebrate with you when you were happy. As an adult you can give those spaces to yourself and invite safe people into them with you.
None of us had perfect parents. So, we all have work to do to learn how to love ourselves well and the way that we need.
It is hard to parent ourselves well if we don’t know ourselves.
That knowing is an ongoing journey we develop as our needs and wants change.
I wonder what is on your Green Light list? What numbers would be on your scale? And what ingredients are in your mental Health Pie? Which of those ingredients are present right now? Which ones are missing? How could you add just one of those ingredients to your pie this week?
Postscript: In the readable version of this post on Substack you will find helpful links throughout the transcript of what is heard on the audio podcast version. The podcast and Substack is called Letters from a Therapist.
That’s what I have to say today. I am guessing you have something to say, too. Happy to hear it.
If you enjoyed listening today, please consider liking this post wherever you read it or listen to it, subscribing to my Substack and sharing it with someone you think might enjoy it, too. The subscription is free and it would mean so much to me. Thank you!












Share this post